Can Thermal Cameras Detect Underground Animals
As discussed further beneath, scientific studies support that certain telethermographic systems, also known as thermal imaging systems, may exist used to measure surface pare temperature. These systems include an infrared thermal photographic camera and may take a temperature reference source. In this certificate, they are referred to equally thermal imaging systems.
Thermal imaging systems and not-contact infrared thermometers (NCITs) use unlike forms of infrared technology to measure temperature. For information about NCITs, delight refer to the fact canvas on Non-contact Infrared Thermometers.
Thermal Imaging Systems and COVID-19
- When used correctly, thermal imaging systems generally have been shown to accurately measure out someone's surface pare temperature without being physically shut to the person being evaluated. Thermal imaging systems offer certain benefits in that other methods need a closer proximity or contact to measure temperature (for example, non-contact infrared thermometers or oral thermometers).
- Temperature-based screening, such as thermal imaging, is non effective at determining if someone definitively has COVID-19 because, among other things, a person with COVID-19 may not have a fever. A diagnostic test must be performed to determine if someone has COVID-19.
- Thermal imaging systems have non been shown to be accurate when used to take the temperature of multiple people at the same time. The accurateness of these systems depends on careful set-upward and operation, too as proper preparation of the person being evaluated.
- Thermal imaging systems have been used by several countries during epidemics, although information nearly their effectiveness as part of efforts to reduce the spread of disease has been mixed.
- The FDA issued the Enforcement Policy for Telethermographic Systems During the Coronavirus Disease 2019 (COVID-nineteen) Public Health Emergency guidance to help expand the availability of thermal imaging systems and mitigate thermometer shortages during the public health emergency. The guidance sets forth an enforcement policy that is intended to apply to all thermal imaging systems that are intended for medical purposes for the duration of the public health emergency related to COVID-19, and provides recommendations regarding functioning and labeling of such systems.
Figure 1 demonstrates the proper thermal imaging setup for processing of individual people in a public expanse.
Benefits of Thermal Imaging Systems
- The person who handles the thermal imaging arrangement is not required to be physically shut to the person existence evaluated. In fact, the person who handles the thermal imaging system could be in a different area or room.
- The thermal imaging system may measure surface skin temperature faster than the typical forehead or oral (mouth) thermometer that requires a close distance or physical contact with the person being evaluated.
- Scientific studies bear witness that, when used correctly, thermal imaging systems generally measure surface pare temperature accurately.
Limitations of Thermal Imaging Systems
- Although these systems may be in use for initial temperature assessment to triage individuals in high throughput areas (for example, airports, businesses and sporting events), the systems have not been shown to exist effective when used to take the temperature of multiple people at the same time. They should not be used for "mass temperature screening."
- These systems mensurate surface pare temperature, which is usually lower than a temperature measured orally. Thermal imaging systems must be adapted properly to right for this departure in measurements.
- These systems work effectively only when all the following are true:
- The systems are used in the right environment or location.
- The systems are set upwardly and operated correctly.
- The person being assessed is prepared according to instructions.
- The person handling the thermal imaging system is properly trained.
Proper Utilise of Thermal Imaging Systems
The person who handles the system should follow all manufacturer instructions to make sure the system is fix properly and located where it can measure surface skin temperature accurately.
The person who handles the organization should be trained to properly gear up both the location where the system will be used, and the person beingness evaluated, to increase accuracy. For details, see the standards and scientific papers listed under References below.
Preparing the Expanse where You lot will Utilize a Thermal Imaging System
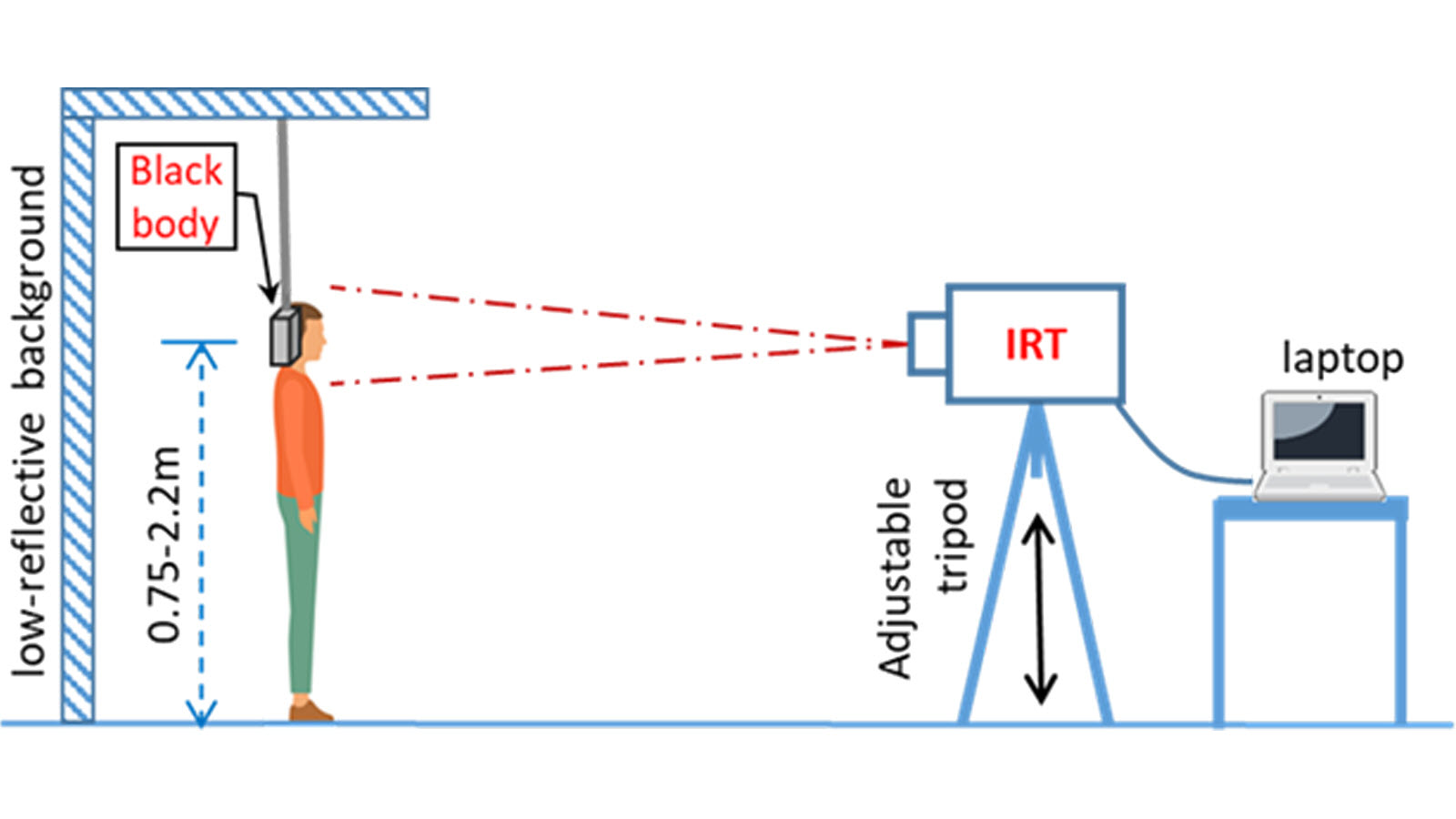
- Room temperature should be 68-76 °F (xx-24 °C) and relative humidity 10-fifty percentage.
- Effort to control other items that could impact the temperature measurement:
- Avert reflective backgrounds (for case, glass, mirrors, metallic surfaces) to minimize reflected infrared radiation.
- Employ in a room with no typhoon (movement of air), out of direct sunlight and away from radiant heat (for case, portable heaters, electrical sources).
- Avoid strong lighting (for example, incandescent, halogen and quartz tungsten halogen light bulbs).
Effigy 2 demonstrates the proper thermal imaging room setup.
Preparing the Thermal Imaging System
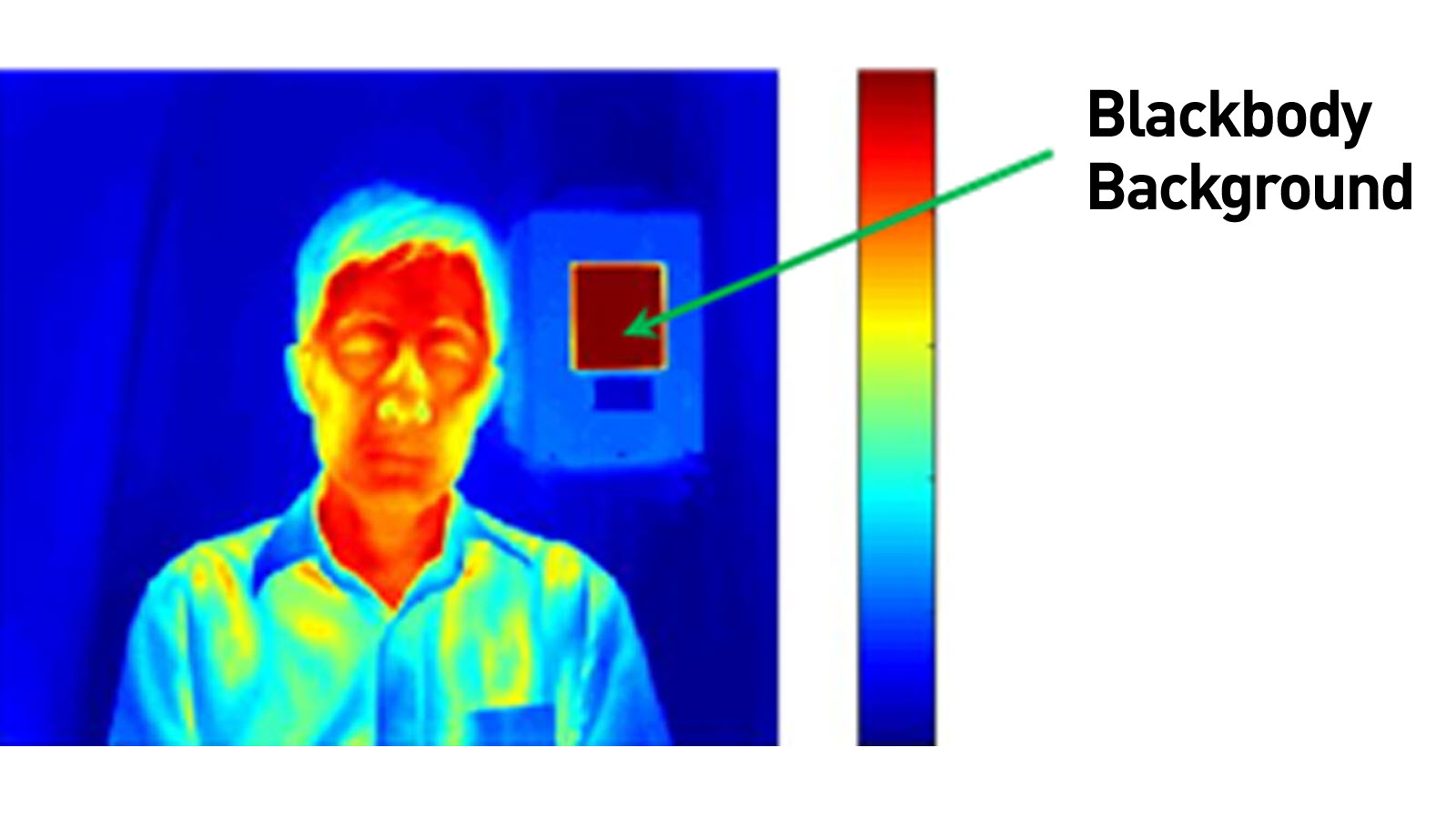
- Some systems crave the utilize of a calibrated blackbody (a tool for checking the scale of an infrared temperature sensor) during evaluation to make sure measurements are accurate. Check the manufacturer'southward instructions to determine if a calibrated blackbody is needed. Some devices do not require i.
- Plough on the entire system 30 minutes before utilise to warm information technology up.
Preparing the Person Being Evaluated
The person treatment the system should make sure the person being evaluated:
- Does not accept whatever face obstructions before measurement, such as a hat, scarf, glasses, or face shield. The person's pilus should be pulled away from their face, and their face should exist clean and dry out. During the COVID-nineteen public health emergency, the FDA believes that the benefits of wearing a mask over the rima oris and olfactory organ while using thermal imaging systems outweighs any potential risk of inaccurate measurements.
- Does not have a higher or lower face temperature from wearing excessive wearable or caput covers (for example, headbands, bandanas) or from using facial cleansing products (for example, cosmetic wipes).
- Has waited at least fifteen minutes in the measurement room or 30 minutes later exercising, strenuous physical activity, bathing, or using hot or cold compresses on the face.
Effigy 3 demonstrates the proper thermal imaging setup for processing of private people using a calibrated blackbody background.
Using the Thermal Imaging Arrangement
- Measure only one person's surface peel temperature at a fourth dimension.
- Position the person at a fixed distance (follow the manufacturer's instructions for employ) from the thermal imaging system, directly facing the camera.
- The paradigm area should include the person's whole face up and the calibrated blackbody, if using one.
- If an increased temperature is seen using the thermal imaging system, you should employ a different method to confirm a fever. Public health officials can help you determine if the fever is a sign of infection.
Questions about Using Thermal Imaging Systems during COVID-19
Q: Are thermal imaging systems effective for screening people for fevers in places like nursing homes, airports, and infirmary emergency rooms?
A: When using a thermal imaging arrangement, it is important to assess whether the arrangement will provide the intended results in high throughput areas. We understand that these devices are beingness used for initial temperature assessment and triage of individuals for elevated temperatures in medical and not-medical environments. They should not be used for measuring temperatures of many people at the same time in crowded areas, in other words "mass temperature screening" is non recommended.
Based on where the system will be used, there may exist more appropriate methods to initially appraise and triage people, especially if there is a risk that infected people would not exist identified correct away. For example:
- In a nursing dwelling, inaccurate temperature measurement or a missed contagious person without a fever could spread infection amidst nursing home residents. And so, in this case, other assessment options and post-obit infection control practices may be more effective.
- In airports, workplaces, grocery stores, concert venues, or other areas where y'all are trying to screen large groups of people for mass temperature screening, diagnostic testing may be too difficult because of the time and costs needed to screen and get results. These systems will probable miss well-nigh individuals with COVID-19 who are contagious. Thermal imaging systems could be considered as one method for initial temperature cess in these types of settings when used as part of a larger approach to risk management.
- In a hospital emergency room, a thermal imaging organization may aid to quickly appraise temperature and triage patients to determine who needs more than evaluation or isolation.
Q: Are thermal imaging systems effective as the sole means of diagnosing COVID-nineteen?
A: No. A fever or higher body temperature is merely one possible symptom of a COVID-19 infection. Thermal imaging systems by and large detect a loftier body temperature accurately when used appropriately. They practice non discover whatsoever other infection symptoms, and many people with COVID-xix can be contagious without a fever. Also, a high trunk temperature does non necessarily mean a person has a COVID-xix infection.
All fevers measured by thermal imaging systems should be confirmed by another method and followed by more diagnostic evaluations for other symptoms, as advisable.
Q: How tin thermal imaging systems help with the COVID-nineteen response?
A: To aid accost urgent public health concerns raised past shortages of temperature measurement products and expand the availability of telethermographic systems used for initial torso temperature for triage apply during this COVID-19 public health emergency, the FDA is applying regulatory flexibility for certain telethermographic systems as outlined in its enforcement policy.
When a high trunk temperature is identified by thermal imaging, an additional evaluation should follow (for example, physician evaluations or interview, laboratory testing and patient observation).
Q: Are thermal imaging systems used for body temperature assessment considered medical devices?
A: Every bit discussed in the enforcement policy, telethermographic systems are devices when they are intended for a medical purpose. To make up one's mind if these products are intended for a medical purpose, FDA will consider whether:
- They are labeled or otherwise intended for apply by a health care professional;
- They are labeled or otherwise for use in a health care facility or environment; and
- They are labeled for an intended use that meets the definition of a device, for example, trunk temperature measurement for diagnostic purposes, including in non-medical environments.
Q: How does a thermal imaging system differ from a thermometer?
A: Both thermal imaging systems and non-contact infrared thermometers (NCIT) tin can mensurate surface temperatures without contact. An NCIT measures surface temperature in a unmarried location, whereas a thermal imaging organisation can measure temperature differences across multiple locations, creating a relative temperature map of a region of the body. The enforcement policy in the guidance applies to utilize of thermal imaging systems to determine initial torso temperature measurements.
In that location is a separate enforcement policy that applies to certain NCITs and other clinical electronic thermometers: Enforcement Policy for Clinical Electronic Thermometers During the Coronavirus Disease 2019 (COVID-19) Public Wellness Emergency.
References
Note, this information is applicable to thermal imaging systems that are intended for a medical purpose. This means that the system is intended for use in the diagnosis of illness or other conditions, or in the cure, mitigation, treatment or prevention of disease and, therefore, meets the definition of "device" set forth in Section 201(h) of the Federal Nutrient, Drug, and Cosmetic Act.
For more information on FDA's policies for these devices, and recommendations on their design, labeling, and apply during the COVID-nineteen Public Health Emergency, please review the following:
Enforcement Policy for Telethermographic Systems During the Coronavirus Disease 2019 (COVID-19) Public Health Emergency: Guidance for Industry and Nutrient and Drug Administration Staff
Additional data on these devices can be found at:
IEC 80601-2-59: Medical electrical equipment - Office 2-59: Particular requirements for bones safety and essential functioning of screening thermoghraphs for human febrile temperature screening. 2017, International Electrotechnical Committee & International Organization for Standardization.
ISO/TR 13154: Medical electrical equipment — Deployment, implementation and operational guidelines for identifying febrile humans using a screening thermograph. 2017, International Arrangement for Standardization.
Ghassemi, P., et al. (2018). "All-time practices for standardized functioning testing of infrared thermographs intended for fever screening." PLoS I 13(9): e0203302.
Source: https://www.fda.gov/medical-devices/general-hospital-devices-and-supplies/thermal-imaging-systems-infrared-thermographic-systems-thermal-imaging-cameras
Posted by: chandlerhostall.blogspot.com


0 Response to "Can Thermal Cameras Detect Underground Animals"
Post a Comment